Body Mass Index In Children With Autism And Typical Controls
ADVERTISEMENT
Body Mass Index in Children with Autism and Typical Controls
Body Mass Index in Children with Autism and Typical Controls
C.J. Newschaffer, L-C. Lee
Center for Autism and Developmental Disabilities Epidemiology, Department of Epidemiology, Johns Hopkins University Bloomberg School of Public Health, Baltimore, MD
Background
Results
Background
Results
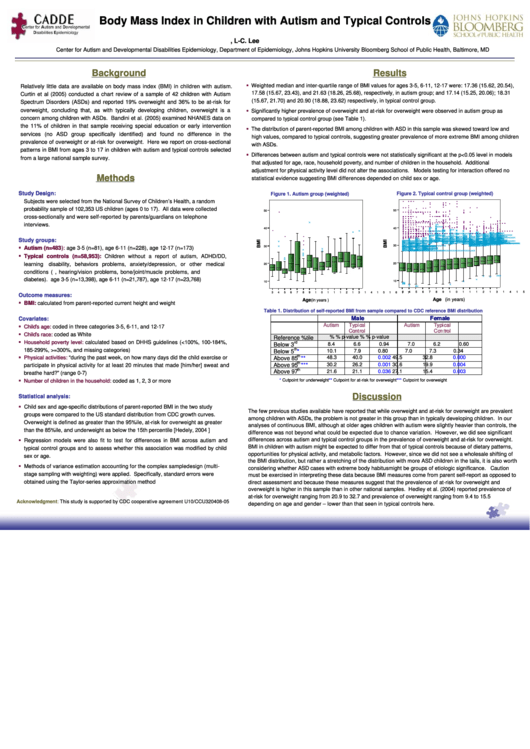
Weighted median and inter-quartile range of BMI values for ages 3-5, 6-11, 12-17 were: 17.36 (15.62, 20.54),
Relatively little data are available on body mass index (BMI) in children with autism.
17.58 (15.67, 23.43), and 21.63 (18.26, 25.68), respectively, in autism group; and 17.14 (15.25, 20.06); 18.31
Curtin et al (2005) conducted a chart review of a sample of 42 children with Autism
(15.67, 21.70) and 20.90 (18.88, 23.62) respectively, in typical control group.
Spectrum Disorders (ASDs) and reported 19% overweight and 36% to be at-risk for
overweight, concluding that, as with typically developing children, overweight is a
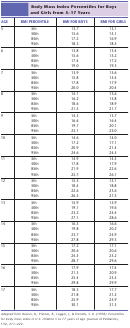
Significantly higher prevalence of overweight and at-risk for overweight were observed in autism group as
concern among children with ASDs. Bandini et al. (2005) examined NHANES data on
compared to typical control group (see Table 1).
the 11% of children in that sample receiving special education or early intervention
The distribution of parent-reported BMI among children with ASD in this sample was skewed toward low and
services (no ASD group specifically identified) and found no difference in the
high values, compared to typical controls, suggesting greater prevalence of more extreme BMI among children
prevalence of overweight or at-risk for overweight. Here we report on cross-sectional
with ASDs.
patterns in BMI from ages 3 to 17 in children with autism and typical controls selected
Differences between autism and typical controls were not statistically significant at the p<0.05 level in models
from a large national sample survey.
that adjusted for age, race, household poverty, and number of children in the household. Additional
adjustment for physical activity level did not alter the associations. Models testing for interaction offered no
Methods
Methods
statistical evidence suggesting BMI differences depended on child sex or age.
Study Design:
Study Design:
Figure 1. Autism group (weighted)
Figure 2. Typical control group (weighted)
Subjects were selected from the National Survey of Children’s Health, a random
V
V V
V V V
V
V
V
V V
V
V
V
V V V
V
V
V
V
V
V V
V
V V
V
V
probability sample of 102,353 US children (ages 0 to 17). All data were collected
V V
V
V V
50
V
50
V
V V V V V V V V V V V V
V V V V V V
V
V
V V V
V V
V
V
V
V
V
V
V V
V
V
V V V
V V V
V
V V V V V V
V V
V V V V V
V V
V V V
cross-sectionally and were self-reported by parents/guardians on telephone
V
V
V
V V V
V
V V V
V
V V
V
V
V
V V V V
V
V V V V V V
V
V
V
V V V V
V V V
V V V
V V V V V V V V
V
V V V
V
V
V V
V
V V
V
V V V V V V V V V V V V V V V V V V V V V V V V V
V V V V V
V V
V
V
R
V V V V V
V V
V V
V
V V V V
V
V V V
interviews.
V V V V
V V V V V
V V
V V
R R
V
V
V
V V
V V V V
V
V V V
V V V V V V
V
V V V
V V V V
V V
V V
V V
V V
R
V
V V V
V V
V V
V V
V V V
R R R R R R
V V V V
V V V V
V V V V V V V
V V V
V V V
R R
V V V V
V
V
V V V V V V V V
V
40
V
V V V V V V
V
V V
R
R
R R
V V V V
40
V V V V V
R R
R R
V V V
V V
V V V
V
R R R
R R R R
V
V
V V V V V V V V V V V
V V V V V
R R
V
V V V V V V V V
R
V V V V V V
R
R R R R
R R R R
R R
R R
V V
V V V V
R R R R R R R R R R R
V V V V
R
V V V V V V V
V V
V V V V V V V V
V
R
R
R R R
R R
R R
R R R R
V V
V V V V V V V V V V V V V V V V V V V V V
V
V
R R R
R R R R R
R
V
V V V V V
R R R R R R R R R
R R R R R R R
V V V V
R R
R R R R R
R R R R R R
R R R R R R R R R
R R R R R R R R
R R
R R R R R R R R R
R R R R R R
R R R R R R
V V V
V V V V V V
R R R R R R R R R R
R R
V V V V V V V V V V V
V V V V V V V V
R R R R
R R R R R R R R
R R
R
R R R R
R
R R
R R R R R R R R R R
R R
R R
R R R R R R R R R R R
V
V
V V V V
V
R R R R
R R R
R R R R R
R R R
R R R R R R
R R R R
R R R R
R R R R R R R
R
R R R
R R R R R R
R R R R R R
R R R R R R R
R R R R R R
R R R R R R R
R R R R R R
R R R R R R R R R R
R R R R R R R R R R R R R R
V
V V V V V V V V V
V V
V V V V V V
R R
R R R R
R R R R R R
R R R R R R R R R
R R R R R R R R R R R
R R R R
R
R R R
R R R
R R R
R
R R R R R R
R R R R
R R R R R R R
R R R R R R
R R R R R R R R R
R R R R R R R R
R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R R R
R
R R R R R R R R R R R R R R R R R R
R R R R
R R R
R R R R R R R R R
R R
R R R R R R R R R R
R R
R
R R R
R
R
R R
R
R R R R R R R R R
R R R R R R R R R R R R
R R
R
R R R R R R R R R R
R R R R R R R R R R R R R
R R R R R R R R R R R R R
R R
R R R R R R R R R
Study groups:
Study groups:
R R
R R R R
R R R R R R R
R R R R
R R R
R R R R R R R
R R R R R R R R R R
R R R R R R R R
R R R R R
R R R R R R R R R R R
R R R R R R R R R R R R
R R R R R R R R R R R R R
V
R R R R R
R
R R R R R R R R R R R
R R R
R R R
R R R R R R R R R R R
R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R R R R R R R
R R R R R R R R R R
R R R R R R R R R R R R R R
R R R R R R R R R
R R R R R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R R R R R
R
R
R R R R R R R R R R R
R R R
R R R R R R R R R R R R R R R R R R
R R R R R R R R R R R R
R
R R R
R
R R R R R R R R R
R R R R
R R R R R R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R
R R R R R R
R
R
R
R R R R R
R R R R R R
R R R R R R R R R R R
R R R R R R R R R
R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R R R R R
R R R R R R R R R
R R R R R R R R R R R
R R R R R R
R R R R R R
R R R R R R R R
R R R R R R R R R
R R R
R R R R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R
R R R R R R R R R R R R
R R R R R R R R R R R R
R R R R R R
R R R R R R R R R R R R R R R R R R R
R
R R R R R R R R R R R R R R R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R R R R R R R R R R R R R R
R R R R R R
R R
R R R R R R R
R R R R R
R R R R R R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R R R R R R R R R R R R R
V
R R R R R R R R R
R R R R
R
R R R R
R R R
R R R R
R R
R R R R R R R
R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R R R R R
R R
R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R
R R R R R R
R R R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R
R
30
R R R R R R R R
30
R
R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R
Autism
(n=483):
):
R R R R R R R R R R R R R R R
R R R R R R
R R R R R R R R R
R R R R R R R R R R R R R R R R
Autism (n=483
age 3-5 (n=81), age 6-11 (n=228), age 12-17 (n=173)
R R R R R
R
R R R R R R R R
R R R R R R R R R R R R R R R R R R R R
R R R R R R R R R R R R R R R R
R R R R
R R R R R R R R R R R R
R R R R
R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R
R R R R R
R
R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R R
R
R
R
R
R
Typical controls (n=58,953):
Typical controls (n=58,953):
Children without a report of autism, ADHD/DD,
R
R
learning
disability, behaviors problems, anxiety/depression, or other medical
20
20
conditions (e.g. asthma, hearing/vision problems, bone/joint/muscle problems, and
R R R
R
R
diabetes). age 3-5 (n=13,398), age 6-11 (n=21,787), age 12-17 (n=23,768)
R
10
R
10
R R
R R R R
R
R
R
R R R
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
Outcome measures:
Outcome measures:
Age (in years)
Age
(in years )
BMI:
BMI:
calculated from parent-reported current height and weight
Table 1.
Distribution of self-reported BMI from sample compared to CDC reference BMI distribution
M
a
l
e
F
e
m
a
l
e
Covariates:
Covariates:
M
a
l
e
F
e
m
a
l
e
A
u
t
i
s
m
T
y
p
i
c
a
l
A
u
t
i
s
m
T
y
p
i
c
a
l
A
u
t
i
s
m
T
y
p
i
c
a
l
A
u
t
i
s
m
T
y
p
i
c
a
l
Child’
’
s age:
coded in three categories 3-5, 6-11, and 12-17
Child
s age:
C
C
o
o
n
n
t
t
r
r
o
o
l
l
C
C
o
o
n
n
t
t
r
r
o
o
l
l
Child’
’
s race:
coded as White v.s. Others
Child
s race:
Reference %tile
%
%
p-value
%
%
p-value
Household poverty level:
calculated based on DHHS guidelines (<100%, 100-184%,
Household poverty level:
rd
Below 3
8.4
6.6
0.94
7.0
6.2
0.60
185-299%, >=300%, and missing categories)
th
Below 5
*
10.1
7.9
0.80
7.0
7.3
0.34
th
Physical activities:
Physical activities:
“during the past week, on how many days did the child exercise or
Above 85
**
48.3
40.0
0.002
49.5
32.8
0.000
th
30.2
26.2
0.001
30.6
19.9
0.004
Above 95
***
participate in physical activity for at least 20 minutes that made [him/her] sweat and
th
Above 97
21.6
21.1
0.036
27.1
15.4
0.003
breathe hard?” (range 0-7)
coded as 1, 2, 3 or more
*
Cutpoint for underweight
**
Cutpoint for at-risk for overweight
***
Cutpoint for overweight
Number of children in the household:
Number of children in the household:
Discussion
Discussion
Statistical analysis:
Statistical analysis:
Child sex and age-specific distributions of parent-reported BMI in the two study
The few previous studies available have reported that while overweight and at-risk for overweight are prevalent
groups were compared to the US standard distribution from CDC growth curves.
among children with ASDs, the problem is not greater in this group than in typically developing children. In our
Overweight is defined as greater than the 95%ile, at-risk for overweight as greater
analyses of continuous BMI, although at older ages children with autism were slightly heavier than controls, the
than the 85%ile, and underweight as below the 15th percentile [Hedely, 2004 ]
difference was not beyond what could be expected due to chance variation. However, we did see significant
differences across autism and typical control groups in the prevalence of overweight and at-risk for overweight.
Regression models were also fit to test for differences in BMI across autism and
BMI in children with autism might be expected to differ from that of typical controls because of dietary patterns,
typical control groups and to assess whether this association was modified by child
opportunities for physical activity, and metabolic factors. However, since we did not see a wholesale shifting of
sex or age.
the BMI distribution, but rather a stretching of the distribution with more ASD children in the tails, it is also worth
Methods of variance estimation accounting for the complex sample design (multi-
considering whether ASD cases with extreme body habitus might be groups of etiologic significance. Caution
stage sampling with weighting) were applied. Specifically, standard errors were
must be exercised in interpreting these data because BMI measures come from parent self-report as opposed to
obtained using the Taylor-series approximation method
direct assessment and because these measures suggest that the prevalence of at-risk for overweight and
overweight is higher in this sample than in other national samples. Hedley et al. (2004) reported prevalence of
at-risk for overweight ranging from 20.9 to 32.7 and prevalence of overweight ranging from 9.4 to 15.5
Acknowledgment:
This study is supported by CDC cooperative agreement U10/CCU320408-05
depending on age and gender – lower than that seen in typical controls here.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1