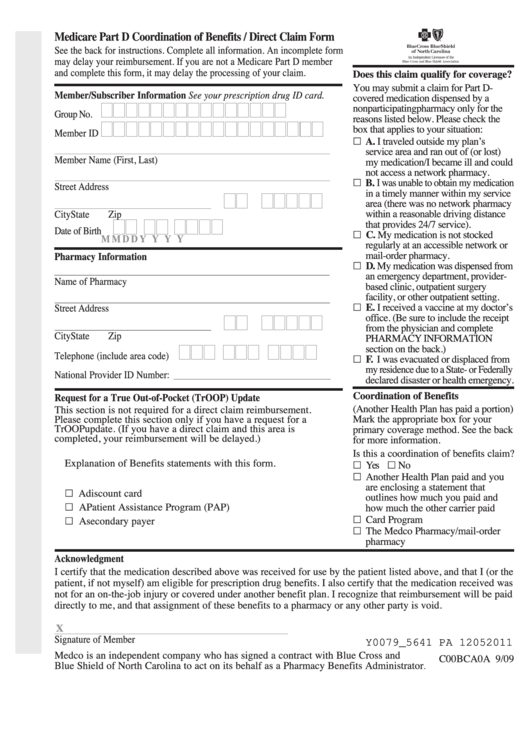
Medicare Part D Coordination of Benefits / Direct Claim Form
See the back for instructions. Complete all information. An incomplete form
may delay your reimbursement. If you are not a Medicare Part D member
and complete this form, it may delay the processing of your claim.
Does this claim qualify for coverage?
You may submit a claim for Part D-
Member/Subscriber Information See your prescription drug ID card.
covered medication dispensed by a
nonparticipatingpharmacy only for the
Group No.
reasons listed below. Please check the
box that applies to your situation:
Member ID
„
A. I traveled outside my plan’
s
service area and ran out of (or lost)
Member Name (First, Last)
my medication/I became ill and could
not access a network pharmacy.
„
B. I was unable to obtain my medication
Street Address
in a timely manner within my service
area (there was no network pharmacy
within a reasonable driving distance
City
State
Zip
that provides 24/7 service).
Date of Birth
„ C. My medication is not stocked
M M
D D
Y Y Y Y
regularly at an accessible network or
mail-order pharmacy.
Pharmacy Information
„ D. My medication was dispensed from
an emergency department, provider-
Name of Pharmacy
based clinic, outpatient surgery
facility, or other outpatient setting.
„ E. I received a vaccine at my doctor’s
Street Address
office. (Be sure to include the receipt
from the physician and complete
City
State
Zip
PHARMACY INFORMATION
section on the back.)
Telephone (include area code)
„ F. I was evacuated or displaced from
my residence due to a State- or Federally
National Provider ID Number:
______________________________
declared disaster or health emergency.
Coordination of Benefits
Request for a True Out-of-Pocket (TrOOP) Update
(Another Health Plan has paid a portion)
This section is not required for a direct claim reimbursement.
Please complete this section only if you have a request for a
Mark the appropriate box for your
TrOOP update. (If you have a direct claim and this area is
primary coverage method. See the back
completed, your reimbursement will be delayed.)
for more information.
1. Please include all applicable pharmacy receipts and/or
Is this a coordination of benefits claim?
„ Yes „ No
Explanation of Benefits statements with this form.
„ Another Health Plan paid and you
2. Check off which of the payers below paid your claim.
are enclosing a statement that
„ A discount card
outlines how much you paid and
„ A Patient Assistance Program (PAP)
how much the other carrier paid
„ Card Program
„ A secondary payer
„ The Medco Pharmacy/mail-order
3. Complete the Other Coverage Section on the back of this form.
pharmacy
Acknowledgment
I certify that the medication described above was received for use by the patient listed above, and that I (or the
patient, if not myself) am eligible for prescription drug benefits. I also certify that the medication received was
not for an on-the-job injury or covered under another benefit plan. I recognize that reimbursement will be paid
directly to me, and that assignment of these benefits to a pharmacy or any other party is void.
X
Signature of Member
Y0079_5641 PA 12052011
Medco is an independent company who has signed a contract with Blue Cross and
C00BCA0A 9/09
Blue Shield of North Carolina to act on its behalf as a Pharmacy Benefits Administrator
.
 1
1 2
2








