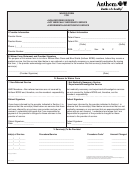
Form 1894 - Anthem Waiver Form For Non-Referred Service/not Medically Necessary Service/experimental/investigative Service
ADVERTISEMENT
WAIVER FORM
FOR
• NON-REFERRED SERVICE
• NOT MEDICALLY NECESSARY SERVICE
• EXPERIMENTAL/INVESTIGATIVE SERVICE
I. Provider Information
II. Patient Information
Provider Name: _______________________________________
Patient Name: ________________________________________
Practice Name: _______________________________________
Medical Necessity
Patient ID#: __________________________________________
(Prefix)
(Suffix)
Phone: (_____)_______________________________________
Anthem BCBS pays only for necessary medical and surgical services in keeping
DOB: _____/_____/_____
Sex:
M
F
with accepted and ethical medical practice. Services or items which do not meet
Provider Number: _____________________________________
medical necessity criteria are excluded from coverage. A medically necessary
service is a serv- ice which:
III. Waiver Form Statement and Provider Signature
The purpose of this waiver form is to inform Anthem Blue Cross and Blue Shield (Anthem BCBS) members, before they receive a
1.! is appropriate and necessary for the diagnosis, prevention, or treatment of a
medical service, that the service listed below is non-referred or not medically necessary or experimental/investigative. By signing
covered medical condition;
this form, I, the provider acknowledge and agree that I have explained to the member that the service(s) listed are not a covered
2.! is within standards of good and generally accepted medical practice as
service(s).
reflected by scientific and peer medical literature, and recognized within the
_____________________________________________________
_____________________
organized medical community in the State of New Hampshire;
(Provider Signature)
(Date)
3.! provides for the diagnosis, prevention or treatment of a medical condition that
is (i) not excluded from coverage under the Subscriber Coverage Certificate and
IV. Reason for Waiver Form
(ii) determined by Anthem BCBS, applying Anthem BCBS’s established medical
Non-Referred Service
Not Medically Necessary Service
poli- cies and guidelines, to be covered;
Experimental/Investigative Service
4.! is not primarily for the personal comfort or convenience of the member,
member’s family, physician, or other provider of care;
HMO Members—Non-referred services are not covered by
Not medically necessary and experimental/investigative services
Anthem BCBS and, therefore, are the member’s responsibility.
are not covered by Anthem BCBS and, therefore, are the
5.! is care or treatment which could not have been omitted without adversely
member’s responsibility.
affecting the patient’s condition or the quality of medical care rendered;
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -
6.! is not in excess, in terms of scope, duration, or intensity of the level of care
Patient Signature
Patient Signature
which is needed to provide safe, adequate, and appropriate diagnosis or treatment;
I have been informed by the provider indicated in Section I. in
I have been informed by the provider indicated in Section I. in
7.! is not part of, or associated with, the scholastic education or vocational
advance that the service(s) listed below are services that have
advance that the service(s) listed below are services that are not
education of the member;
not been referred by my primary care provider and are not
medically necessary or are services that are experimental/investi-
8.! is not for investigative or research purposes which are experimental in nature;
covered. I understand and agree that I am responsible for
gative and are not covered. I understand and agree that I am
9.! is not custodial or convalescent care; and 10. in the case of inpatient care,
payment of the provider’s charges for these services to the
responsible for payment of the provider’s charges for these
provider of service.
services to the provider of service.
cannot be provided on an outpatient basis.
If a treatment, service, supply, equipment, or drug does not meet any of the medical
Patient Signature:____________________________________
Patient Signature: ______________________________________
necessity criteria, the treatment, service, supply, equipment, or drug will be
Date: __________________
Date: __________________
considered not medically necessary and will be denied. The member may not be
billed for services denied as not medically necessary unless the member has agreed
V. Service(s) To Be Provided
in advance in writ- ing to pay for such services.
Date(s) of Service
Procedure/Service
Procedure Code*
Amount Charged
_____/_____/_____
_______________________________
______________
_____________
_____/_____/_____
_______________________________
______________
_____________
_____/_____/_____
_______________________________
______________
_____________
_____/_____/_____
_______________________________
______________
_____________
*If applicable
An independent licensee of the Blue Cross and Blue Shield Association.
Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of New Hampshire, Inc.
® Registered marks of the Blue Cross and Blue Shield Association.
1894 (7/01)
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2








