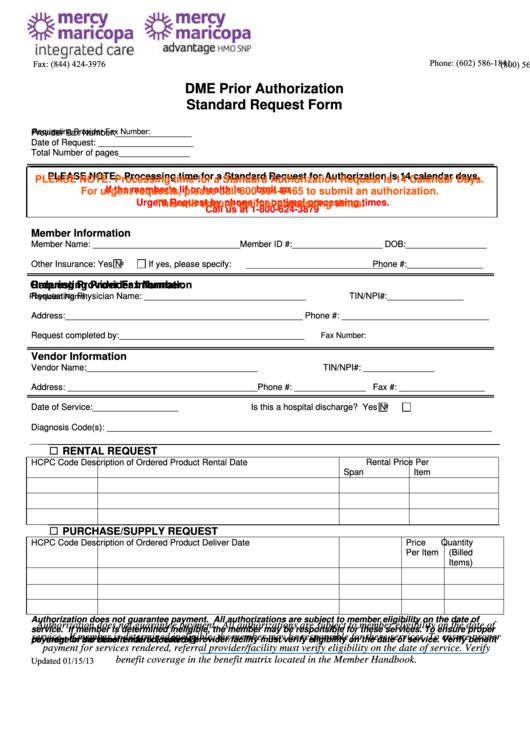
Phone: (602) 586-1841
Fax: (844) 424-3976
(800) 564-5465
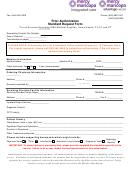
DME Prior Authorization
Standard Request Form
Requesting Provider Fax Number:
Provider Fax Number:________________
Date of Request: ____________________
Total Number of pages_______________
PLEASE NOTE: Processing time for a Standard Request for Authorization is 14 calendar days.
PLEASE NOTE: Processing time for a Standard Authorization Request is 14 Calendar Days.
If the member’s lif or health is
bmit an
For urgent requests, please call 800-564-5465 to submit an authorization.
Urgent Request by phone for optimal processing times.
This will ensure optimal processing times.
Call us at 1-800-624-3879
Member Information
Member Name: _______________________________Member ID #:___________________ DOB:_________________
Other Insurance: Yes
No
If yes, please specify:
Phone #:________________
Ordering Provider Fax Number:
Requesting Provider Information
Requesting Physician Name: __________________________________
TIN/NPI#:________________
Physician Name:
Address:__________________________________________________ Phone #: _______________________________
Request completed by:_______________________________________
Fax Number:
Vendor Information
Vendor Name:____________________________________
TIN/NPI#: _______________
Address: ________________________________________Phone #: _______________
Fax #: __________________
Date of Service:__________________
Is this a hospital discharge? Yes
No
Diagnosis Code(s): _________________________________________________________________________________
RENTAL REQUEST
HCPC Code
Description of Ordered Product
Rental Date
Rental Price Per
Span
Item
PURCHASE/SUPPLY REQUEST
HCPC Code
Description of Ordered Product
Deliver Date
Price
Quantity
Per Item
(Billed
Items)
Authorization does not guarantee payment. All authorizations are subject to member eligibility on the date of
Authorization does not guarantee payment. All authorizations are subject to member eligibility on the date of
service. If member is determined ineligible, the member may be responsible for these services. To ensure proper
service. If member is determined ineligible, the member may be responsible for these services. To ensure proper
payment for services rendered, referral provider/facility must verify eligibility on the date of service. Verify benefit
payment for services rendered, referral provider/facility must verify eligibility on the date of service. Verify
coverage in the benefit matrix located @
Updated 01/15/13
benefit coverage in the benefit matrix located in the Member Handbook.
 1
1