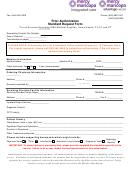
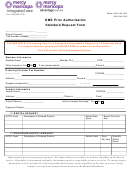
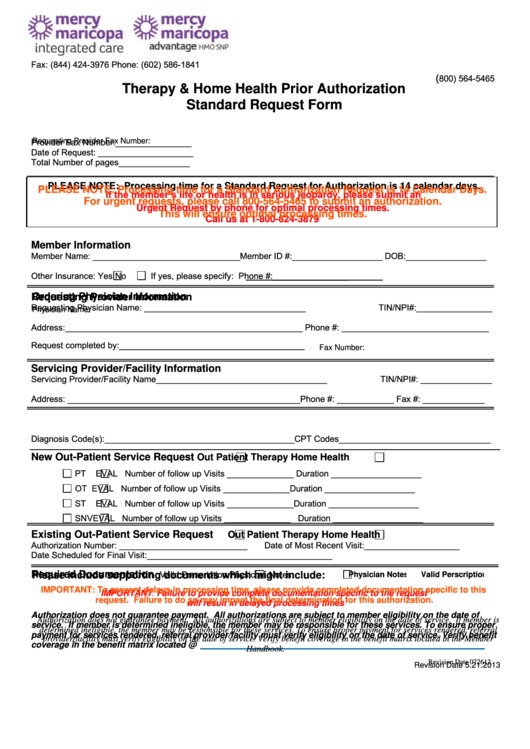
Fax: (844) 424-3976
Phone: (602) 586-1841
(
800) 564-5465
Therapy & Home Health Prior Authorization
Standard Request Form
Provider Fax Number:________________
Requesting Provider Fax Number:
Date of Request: ____________________
Total Number of pages_______________
PLEASE NOTE: Processing time for a Standard Request for Authorization is 14 calendar days.
PLEASE NOTE: Processing time for a Standard Authorization Request is 14 Calendar Days.
If the member’s life or health is in serious jeopardy, please submit an
For urgent requests, please call 800-564-5465 to submit an authorization.
Urgent Request by phone for optimal processing times.
This will ensure optimal processing times.
Call us at 1-800-624-3879
Member Information
Member Name: _______________________________Member ID #:___________________ DOB:_________________
Other Insurance: Yes
No
If yes, please specify:
Phone #:________________
Ordering Physician Information
Requesting Provider Information
Requesting Physician Name: __________________________________
TIN/NPI#:________________
Physician Name:
Address:__________________________________________________ Phone #: _______________________________
Request completed by:_______________________________________
Fax Number:
Servicing Provider/Facility Information
Servicing Provider/Facility Name____________________________________
TIN/NPI#: _______________
Address: _________________________________________________ Phone #: ____________ Fax #: _____________
Diagnosis Code(s):________________________________________CPT Codes________________________________
New Out-Patient Service Request
Out Patient Therapy
Home Health
PT
EVAL Number of follow up Visits ______________ Duration ___________________
OT
EVAL Number of follow up Visits ______________ Duration ___________________
ST
EVAL Number of follow up Visits ______________ Duration ___________________
SNV
EVAL Number of follow up Visits ______________ Duration ___________________
Existing Out-Patient Service Request
Out Patient Therapy
Home Health
Authorization Number: ___________________________
Date of Most Recent Visit:____________________
Date Scheduled for Final Visit: _______________________________________
Valid Prescription
Physician Notes
Required Documentation
Please include supporting documents which might include:
Physician Notes
Valid Perscription
IMPORTANT: To prevent delays in processing time, please provide completed documentation specific to this
IMPORTANT: Failure to provide complete documentation specific to the request
request. Failure to do so may impact the final determination for this authorization.
will result in delayed processing times
Authorization does not guarantee payment. All authorizations are subject to member eligibility on the date of
Authorization does not guarantee payment. All authorizations are subject to member eligibility on the date of service. If member is
service. If member is determined ineligible, the member may be responsible for these services. To ensure proper
determined ineligible, the member may be responsible for these services. To ensure proper payment for services rendered, referral
payment for services rendered, referral provider/facility must verify eligibility on the date of service. Verify benefit
provider/facility must verify eligibility on the date of service. Verify benefit coverage in the benefit matrix located in the Member
coverage in the benefit matrix located @
Handbook.
Revision Date 072612
Revision Date 5.21.2013
 1
1