Form X16156r05 - Provider Claim Adjustment/status Check/appeal Form - Blue Cross Blue Shield Of Minnesota And Blue Plus
ADVERTISEMENT
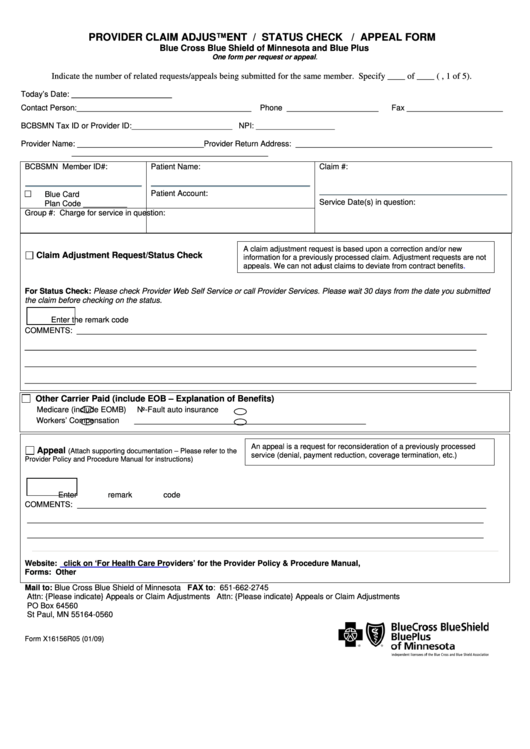
PROVIDER CLAIM ADJUSTMENT / STATUS CHECK / APPEAL FORM
Blue Cross Blue Shield of Minnesota and Blue Plus
One form per request or appeal.
Indicate the number of related requests/appeals being submitted for the same member. Specify ____ of ____ (e.g., 1 of 5).
Today’s Date: _______________________
Contact Person:________________________________________
Phone _____________________
Fax ______________________
BCBSMN Tax ID or Provider ID:_______________________ NPI: __________________
Provider Name: _____________________________Provider Return Address:
_____________________________________________
_____________________________________________
BCBSMN Member ID#:
Patient Name:
Claim #:
□
Patient Account:
Blue Card
Service Date(s) in question:
Plan Code __________
Group #:
Charge for service in question:
A claim adjustment request is based upon a correction and/or new
Claim Adjustment Request/Status Check
information for a previously processed claim. Adjustment requests are not
appeals. We can not adjust claims to deviate from contract
benefits.
For Status Check: Please check Provider Web Self Service or call Provider Services. Please wait 30 days from the date you submitted
the claim before checking on the status.
Enter the remark code
COMMENTS: ______________________________________________________________________________________________
_______________________________________________________________________________________________
_______________________________________________________________________________________________
_______________________________________________________________________________________________
Other Carrier Paid (include EOB – Explanation of Benefits)
Medicare (include EOMB)
No-Fault auto insurance
Workers’ Compensation
_____________________________________________________
An appeal is a request for reconsideration of a previously processed
Appeal
(Attach supporting documentation – Please refer to the
service (denial, payment reduction, coverage termination, etc.)
Provider Policy and Procedure Manual for instructions)
Enter remark code
______________________________________________________________________________________
COMMENTS:
________________________________________________________________________________________________
________________________________________________________________________________________________
Website:
click on ‘For Health Care Providers’ for the Provider Policy & Procedure Manual,
Forms: Other
Mail to: Blue Cross Blue Shield of Minnesota
FAX to: 651-662-2745
Attn: {Please indicate} Appeals or Claim Adjustments
Attn: {Please indicate} Appeals or Claim Adjustments
PO Box 64560
St Paul, MN 55164-0560
Form X16156R05 (01/09)
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2