Patient History Form/history Of Present Illness/past Medical & Social History
ADVERTISEMENT
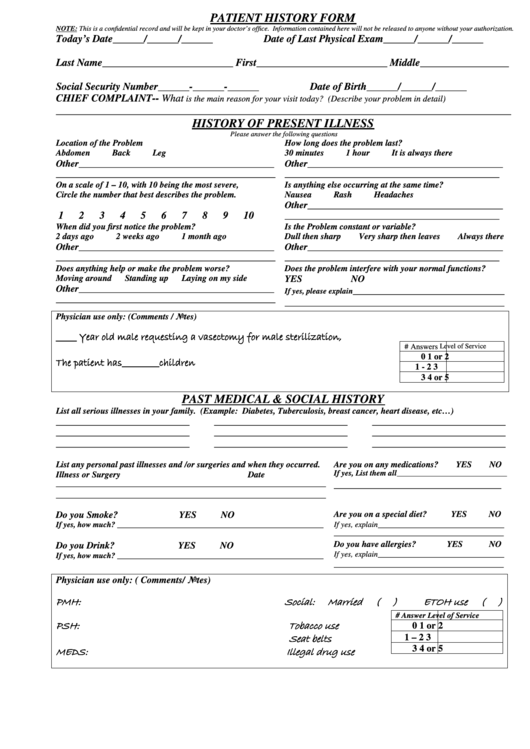
PATIENT HISTORY FORM
NOTE: This is a confidential record and will be kept in your doctor’s office. Information contained here will not be released to anyone without your authorization.
Today’s Date______/______/______
Date of Last Physical Exam______/______/______
Last Name_________________________ First_________________________ Middle_________________
Social Security Number______-______-______
Date of Birth______/______/______
CHIEF COMPLAINT-- What
is the main reason for your visit today? (Describe your problem in detail)
_______________________________________________________________________________________
HISTORY OF PRESENT ILLNESS
Please answer the following questions
Location of the Problem
How long does the problem last?
Abdomen
Back
Leg
30 minutes
1 hour
It is always there
Other_________________________________________
Other_________________________________________
______________________________________________
_____________________________________________
On a scale of 1 – 10, with 10 being the most severe,
Is anything else occurring at the same time?
Circle the number that best describes the problem.
Nausea
Rash
Headaches
Other_________________________________________
1
2
3
4
5
6
7
8
9
10
_____________________________________________
When did you first notice the problem?
Is the Problem constant or variable?
2 days ago
2 weeks ago
1 month ago
Dull then sharp
Very sharp then leaves
Always there
Other_________________________________________
Other_________________________________________
______________________________________________
_____________________________________________
Does anything help or make the problem worse?
Does the problem interfere with your normal functions?
Moving around
Standing up
Laying on my side
YES
NO
Other_________________________________________
_____________________________
If yes, please explain
______________________________________________
__________________________________________
Physician use only: (Comments / Notes)
_____ Year old male requesting a vasectomy for male sterilization,
# Answers
Level of Service
0
1 or 2
The patient has_________children
1 - 2
3
3
4 or 5
PAST MEDICAL & SOCIAL HISTORY
List all serious illnesses in your family. (Example: Diabetes, Tuberculosis, breast cancer, heart disease, etc…)
____________________________
____________________________
____________________________
____________________________
____________________________
____________________________
____________________________
____________________________
____________________________
List any personal past illnesses and /or surgeries and when they occurred.
Are you on any medications?
YES
NO
Illness or Surgery
Date
If yes, List them all
_______________________________
________________________________
______________________________________________________________
______________________________________________________________
Do you Smoke?
YES
NO
Are you on a special diet?
YES
NO
_____________________________
If yes, explain
If yes, how much? _____________________________________________________
_______________________________________
Do you have allergies?
YES
NO
Do you Drink?
YES
NO
_____________________________
If yes, explain
If yes, how much? _____________________________________________________
_______________________________________
Physician use only: ( Comments/ Notes)
PMH:
Social:
Married
(
)
ETOH use
(
)
# Answer
Level of Service
PSH:
Tobacco use
0
1 or 2
Seat belts
1 – 2
3
3
4 or 5
MEDS:
Illegal drug use
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Education
 1
1








