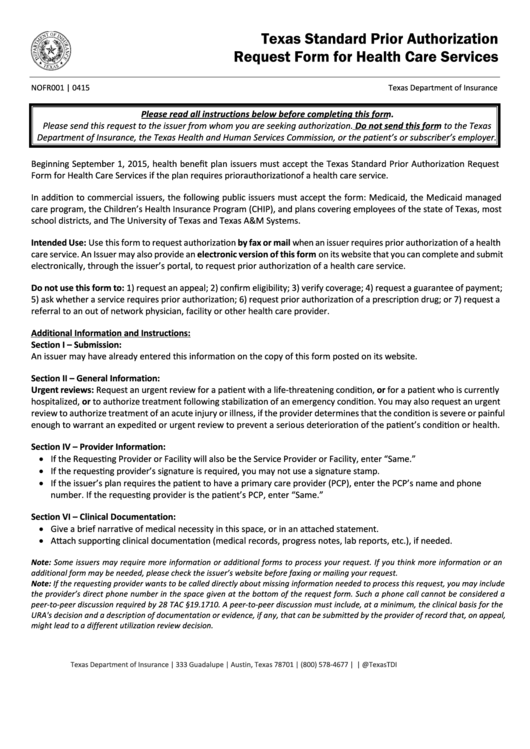
Texas Standard Prior Authorization
Request Form for Health Care Services
NOFR001 | 0415
Texas Department of Insurance
Please read all instructions below before completing this form.
Please send this request to the issuer from whom you are seeking authorization. Do not send this form to the Texas
Department of Insurance, the Texas Health and Human Services Commission, or the patient’s or subscriber’s employer.
Beginning September 1, 2015, health benefit plan issuers must accept the Texas Standard Prior Authorization Request
Form for Health Care Services if the plan requires prior authorization of a health care service.
In addition to commercial issuers, the following public issuers must accept the form: Medicaid, the Medicaid managed
care program, the Children’s Health Insurance Program (CHIP), and plans covering employees of the state of Texas, most
school districts, and The University of Texas and Texas A&M Systems.
Intended Use: Use this form to request authorization by fax or mail when an issuer requires prior authorization of a health
care service. An Issuer may also provide an electronic version of this form on its website that you can complete and submit
electronically, through the issuer’s portal, to request prior authorization of a health care service.
Do not use this form to: 1) request an appeal; 2) confirm eligibility; 3) verify coverage; 4) request a guarantee of payment;
5) ask whether a service requires prior authorization; 6) request prior authorization of a prescription drug; or 7) request a
referral to an out of network physician, facility or other health care provider.
Additional Information and Instructions:
Section I – Submission:
An issuer may have already entered this information on the copy of this form posted on its website.
Section II – General Information:
Urgent reviews: Request an urgent review for a patient with a life-threatening condition, or for a patient who is currently
hospitalized, or to authorize treatment following stabilization of an emergency condition. You may also request an urgent
review to authorize treatment of an acute injury or illness, if the provider determines that the condition is severe or painful
enough to warrant an expedited or urgent review to prevent a serious deterioration of the patient’s condition or health.
Section IV – Provider Information:
• If the Requesting Provider or Facility will also be the Service Provider or Facility, enter “Same.”
• If the requesting provider’s signature is required, you may not use a signature stamp.
• If the issuer’s plan requires the patient to have a primary care provider (PCP), enter the PCP’s name and phone
number. If the requesting provider is the patient’s PCP, enter “Same.”
Section VI – Clinical Documentation:
• Give a brief narrative of medical necessity in this space, or in an attached statement.
• Attach supporting clinical documentation (medical records, progress notes, lab reports, etc.), if needed.
Note: Some issuers may require more information or additional forms to process your request. If you think more information or an
additional form may be needed, please check the issuer’s website before faxing or mailing your request.
Note: If the requesting provider wants to be called directly about missing information needed to process this request, you may include
the provider’s direct phone number in the space given at the bottom of the request form. Such a phone call cannot be considered a
peer-to-peer discussion required by 28 TAC §19.1710. A peer-to-peer discussion must include, at a minimum, the clinical basis for the
URA's decision and a description of documentation or evidence, if any, that can be submitted by the provider of record that, on appeal,
might lead to a different utilization review decision.
Texas Department of Insurance | 333 Guadalupe | Austin, Texas 78701 | (800) 578-4677 | | @TexasTDI
 1
1 2
2