Medical History Form
ADVERTISEMENT
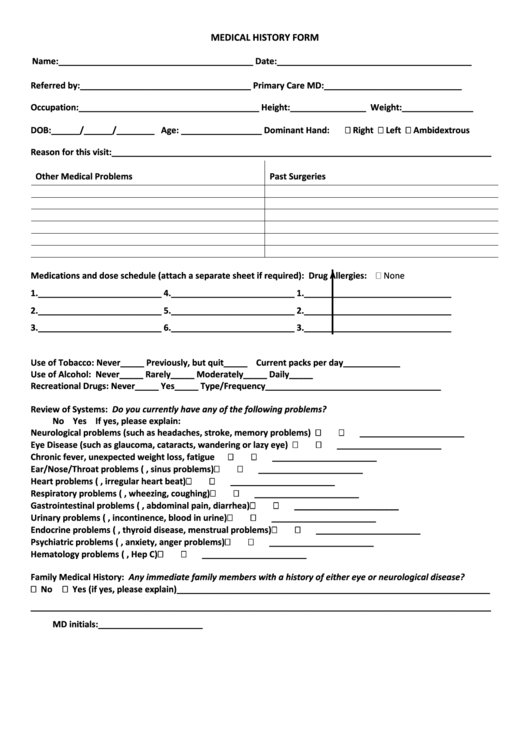
MEDICAL HISTORY FORM
Name:_________________________________________
Date:_________________________________________
Referred by:____________________________________
Primary Care MD:_____________________________
Occupation:______________________________________
Height:________________ Weight:_______________
DOB:______/______/________ Age: _________________
Dominant Hand:
Right
Left
Ambidextrous
Reason for this visit:________________________________________________________________________________
Other Medical Problems
Past Surgeries
Medications and dose schedule (attach a separate sheet if required):
Drug Allergies:
None
1.__________________________
4.__________________________
1._______________________________
2.__________________________
5.__________________________
2._______________________________
3.__________________________
6.__________________________
3._______________________________
Use of Tobacco:
Never_____
Previously, but quit_____
Current packs per day____________
Use of Alcohol:
Never_____
Rarely_____ Moderately_____
Daily_____
Recreational Drugs:
Never_____
Yes_____
Type/Frequency_____________________________________
Review of Systems: Do you currently have any of the following problems?
No Yes If yes, please explain:
Neurological problems (such as headaches, stroke, memory problems)
______________________
Eye Disease (such as glaucoma, cataracts, wandering or lazy eye)
______________________
Chronic fever, unexpected weight loss, fatigue
______________________
Ear/Nose/Throat problems (e.g. hearing loss, sinus problems)
______________________
Heart problems (e.g. chest pain, irregular heart beat)
______________________
Respiratory problems (e.g. shortness of breath, wheezing, coughing)
______________________
Gastrointestinal problems (e.g. heartburn, abdominal pain, diarrhea)
______________________
Urinary problems (e.g. pain, incontinence, blood in urine)
______________________
Endocrine problems (e.g. diabetes, thyroid disease, menstrual problems)
______________________
Psychiatric problems (e.g. depression, anxiety, anger problems)
______________________
Hematology problems (e.g. HIV, Hep C)
______________________
Family Medical History: Any immediate family members with a history of either eye or neurological disease?
No
Yes (if yes, please explain)__________________________________________________________________
_________________________________________________________________________________________________
MD initials:______________________
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1








