New Patient History Form
ADVERTISEMENT
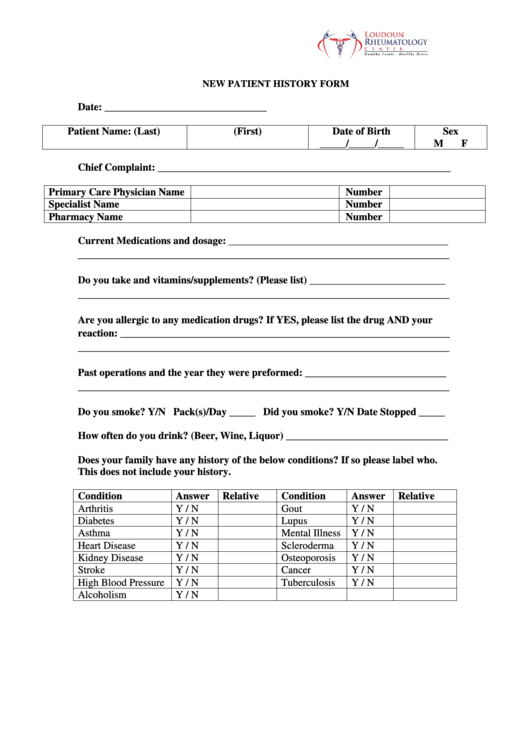
NEW PATIENT HISTORY FORM
Date: _______________________________
Patient Name: (Last)
(First)
Date of Birth
Sex
_____/_____/_____
M
F
Chief Complaint: ________________________________________________________
Primary Care Physician Name
Number
Specialist Name
Number
Pharmacy Name
Number
Current Medications and dosage: __________________________________________
_______________________________________________________________________
Do you take and vitamins/supplements? (Please list) __________________________
_______________________________________________________________________
Are you allergic to any medication drugs? If YES, please list the drug AND your
reaction: _______________________________________________________________
_______________________________________________________________________
Past operations and the year they were preformed: ___________________________
_______________________________________________________________________
Do you smoke? Y/N Pack(s)/Day _____ Did you smoke? Y/N Date Stopped _____
How often do you drink? (Beer, Wine, Liquor) _______________________________
Does your family have any history of the below conditions? If so please label who.
This does not include your history.
Condition
Answer
Relative
Condition
Answer
Relative
Arthritis
Y / N
Gout
Y / N
Diabetes
Y / N
Lupus
Y / N
Asthma
Y / N
Mental Illness
Y / N
Heart Disease
Y / N
Scleroderma
Y / N
Kidney Disease
Y / N
Osteoporosis
Y / N
Stroke
Y / N
Cancer
Y / N
High Blood Pressure
Y / N
Tuberculosis
Y / N
Alcoholism
Y / N
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1