Form Ne-14-06-67 - Aetna Provider Claim Resubmission/reconsideration Form
ADVERTISEMENT
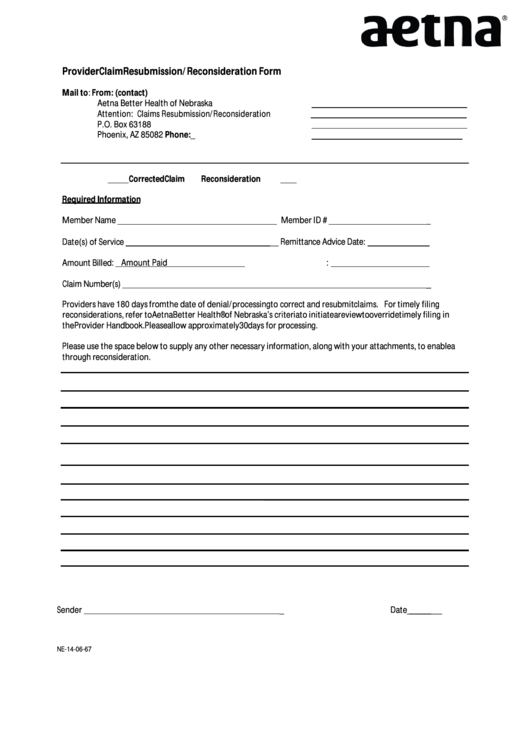
Provider Claim Resubmission /Reconsideration Form
Mail to:
From: (contact)
Aetna Better Health of Nebraska
Attention: Claims Resubmission/Reconsideration
P.O. Box 63188
Phoenix, AZ 85082
Phone:
_
Corrected Claim
Reconsideration
Required Information
Member Name
Member ID #
_
Date(s) of Service
__ Remittance Advice Date:
_
Amount Billed:
Amount Paid:
Claim Number(s)
_
Providers have 180 days from the date of denial/processing to correct and resubmit claims. For timely filing
reconsiderations, refer to Aetna Better Health® of Nebraska’s criteria to initiate a review to override timely filing in
the Provider Handbook. Please allow approximately 30 days for processing.
Please use the space below to supply any other necessary information, along with your attachments, to enable a
through reconsideration.
Sender
_
Date
________
NE-14-06-67
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1








