Form Cf48777 - Prescription Drug Reimbursement Form
ADVERTISEMENT
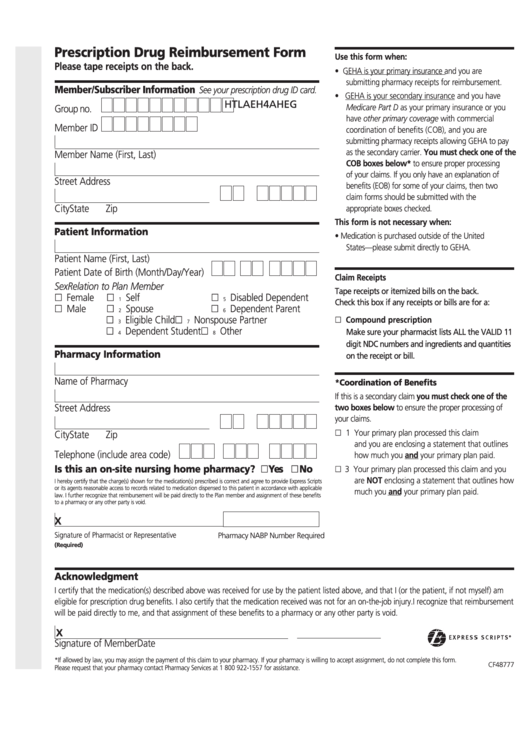
Prescription Drug Reimbursement Form
Use this form when:
Please tape receipts on the back.
• GEHA is your primary insurance and you are
submitting pharmacy receipts for reimbursement.
Member/Subscriber Information
See your prescription drug ID card.
• GEHA is your secondary insurance and you have
G
E
H
A
4
H
E
A
L
T
H
Medicare Part D as your primary insurance or you
Group no.
have other primary coverage with commercial
Member ID
coordination of benefits (COB), and you are
submitting pharmacy receipts allowing GEHA to pay
as the secondary carrier. You must check one of the
Member Name (First, Last)
COB boxes below* to ensure proper processing
of your claims. If you only have an explanation of
Street Address
benefits (EOB) for some of your claims, then two
claim forms should be submitted with the
City
State
Zip
appropriate boxes checked.
This form is not necessary when:
Patient Information
• Medication is purchased outside of the United
States—please submit directly to GEHA.
Patient Name (First, Last)
Patient Date of Birth (Month/Day/Year)
Claim Receipts
Sex
Relation to Plan Member
Tape receipts or itemized bills on the back.
„ Female
„
„
Self
Disabled Dependent
1
5
Check this box if any receipts or bills are for a:
„ Male
„
„
Spouse
Dependent Parent
2
6
„
„
„ Compound prescription
Eligible Child
Nonspouse Partner
3
7
„
Dependent Student „
Other
Make sure your pharmacist lists ALL the VALID 11
4
8
digit NDC numbers and ingredients and quantities
Pharmacy Information
on the receipt or bill.
Name of Pharmacy
*Coordination of Benefits
If this is a secondary claim you must check one of the
Street Address
two boxes below to ensure the proper processing of
your claims.
„ 1 Your primary plan processed this claim
City
State
Zip
and you are enclosing a statement that outlines
Telephone (include area code)
how much you and your primary plan paid.
Is this an on-site nursing home pharmacy? „Yes
„No
„ 3 Your primary plan processed this claim and you
are NOT enclosing a statement that outlines how
I hereby certify that the charge(s) shown for the medication(s) prescribed is correct and agree to provide Express Scripts
or its agents reasonable access to records related to medication dispensed to this patient in accordance with applicable
much you and your primary plan paid.
law. I further recognize that reimbursement will be paid directly to the Plan member and assignment of these benefits
to a pharmacy or any other party is void.
X
Signature of Pharmacist or Representative
Pharmacy NABP Number Required
(Required)
Acknowledgment
I certify that the medication(s) described above was received for use by the patient listed above, and that I (or the patient, if not myself) am
eligible for prescription drug benefits. I also certify that the medication received was not for an on-the-job injury. I recognize that reimbursement
will be paid directly to me, and that assignment of these benefits to a pharmacy or any other party is void.
X
Signature of Member
Date
*If allowed by law, you may assign the payment of this claim to your pharmacy. If your pharmacy is willing to accept assignment, do not complete this form.
CF48777
Please request that your pharmacy contact Pharmacy Services at 1 800 922-1557 for assistance.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1 2
2








