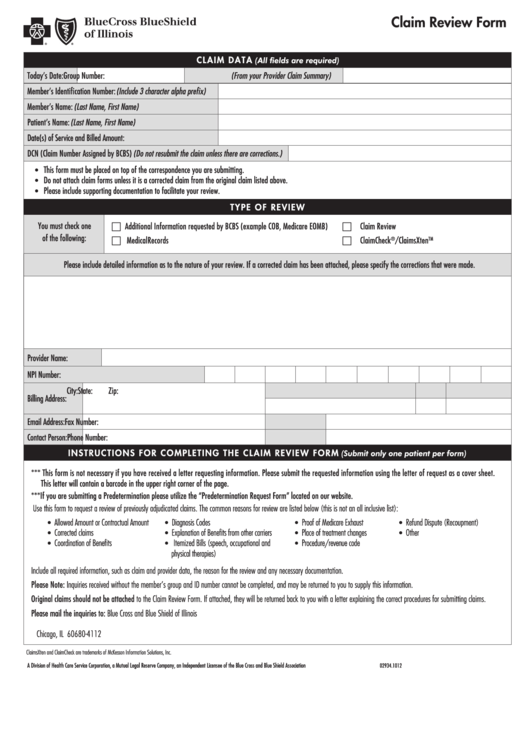
claim Review Form
cl a im data
(All fields are required)
Today’s Date:
Group Number: (From your Provider Claim Summary)
Member’s Identification Number: (Include 3 character alpha prefix)
Member’s Name: (Last Name, First Name)
Patient’s Name: (Last Name, First Name)
Date(s) of Service and Billed Amount:
DCN (Claim Number Assigned by BCBS) (Do not resubmit the claim unless there are corrections.)
This form must be placed on top of the correspondence you are submitting.
•
Do not attach claim forms unless it is a corrected claim from the original claim listed above.
•
Please include supporting documentation to facilitate your review.
•
tY PE OF REVi EW
You must check one
c Additional Information requested by BCBS (example COB, Medicare EOMB)
c Claim Review
of the following:
c Medical Records
c ClaimCheck
/ClaimsXten
®
TM
Please include detailed information as to the nature of your review. If a corrected claim has been attached, please specify the corrections that were made.
Provider Name:
NPI Number:
City:
State:
Zip:
Billing Address:
Email Address:
Fax Number:
Contact Person:
Phone Number:
iNS t RUc t iONS F OR cOm P l Eti NG tH E cl ai m R EViE W FOR m
(Submit only one patient per form)
*** This form is not necessary if you have received a letter requesting information. Please submit the requested information using the letter of request as a cover sheet.
This letter will contain a barcode in the upper right corner of the page.
***If you are submitting a Predetermination please utilize the “Predetermination Request Form” located on our website.
Use this form to request a review of previously adjudicated claims. The common reasons for review are listed below (this is not an all inclusive list):
Allowed Amount or Contractual Amount
Diagnosis Codes
Proof of Medicare Exhaust
Refund Dispute (Recoupment)
•
•
•
•
Corrected claims
Explanation of Benefits from other carriers
Place of treatment changes
Other
•
•
•
•
Coordination of Benefits
Itemized Bills (speech, occupational and
Procedure/revenue code
•
•
•
physical therapies)
Include all required information, such as claim and provider data, the reason for the review and any necessary documentation.
Please Note: Inquiries received without the member’s group and ID number cannot be completed, and may be returned to you to supply this information.
Original claims should not be attached to the Claim Review Form. If attached, they will be returned back to you with a letter explaining the correct procedures for submitting claims.
Please mail the inquiries to:
Blue Cross and Blue Shield of Illinois
P.O. Box 805107
Chicago, IL 60680-4112
ClaimsXten and ClaimCheck are trademarks of McKesson Information Solutions, Inc.
A Division of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield Association
02934.1012
 1
1