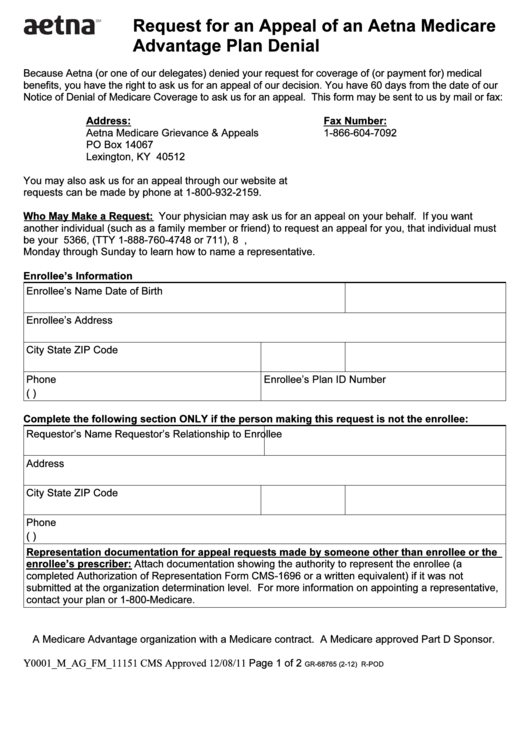
Request for an Appeal of an Aetna Medicare
Advantage Plan Denial
Because Aetna (or one of our delegates) denied your request for coverage of (or payment for) medical
benefits, you have the right to ask us for an appeal of our decision. You have 60 days from the date of our
Notice of Denial of Medicare Coverage to ask us for an appeal. This form may be sent to us by mail or fax:
Address:
Fax Number:
Aetna Medicare Grievance & Appeals
1-866-604-7092
PO Box 14067
Lexington, KY 40512
You may also ask us for an appeal through our website at Expedited appeal
requests can be made by phone at 1-800-932-2159.
Who May Make a Request: Your physician may ask us for an appeal on your behalf. If you want
another individual (such as a family member or friend) to request an appeal for you, that individual must
be your representative. Contact us at 1-800-282-5366, (TTY 1-888-760-4748 or 711), 8 a.m. to 8 p.m.,
Monday through Sunday to learn how to name a representative.
Enrollee’s Information
Enrollee’s Name
Date of Birth
Enrollee’s Address
City
State
ZIP Code
Phone
Enrollee’s Plan ID Number
(
)
Complete the following section ONLY if the person making this request is not the enrollee:
Requestor’s Name
Requestor’s Relationship to Enrollee
Address
City
State
ZIP Code
Phone
(
)
R epresentation documentation for appeal requests made by someone other than enrollee or the
U
enrollee’s prescriber:
Attach documentation showing the authority to represent the enrollee (a
U
completed Authorization of Representation Form CMS-1696 or a written equivalent) if it was not
submitted at the organization determination level. For more information on appointing a representative,
contact your plan or 1-800-Medicare.
A Medicare Advantage organization with a Medicare contract. A Medicare approved Part D Sponsor.
Y0001_M_AG_FM_11151 CMS Approved 12/08/11
Page 1 of 2
GR-68765 (2-12) R-POD
 1
1 2
2