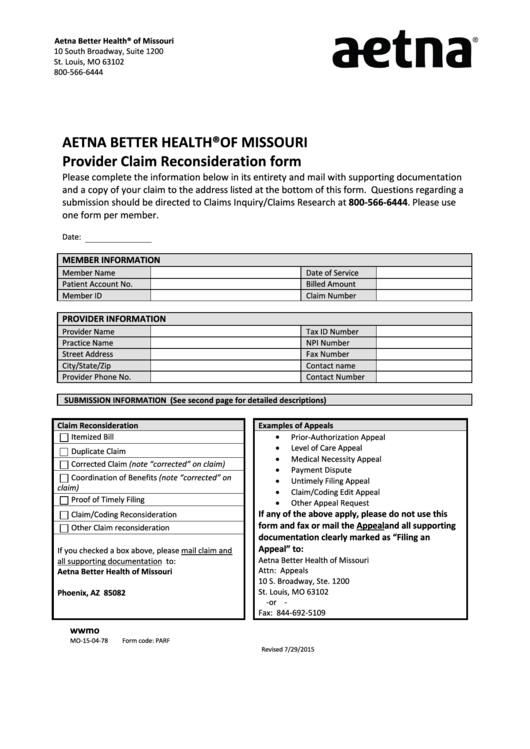
Aetna Better Health® of Missouri
10 South Broadway, Suite 1200
St. Louis, MO 63102
800-566-6444
AETNA BETTER HEALTH® OF MISSOURI
Provider Claim Reconsideration form
Please complete the information below in its entirety and mail with supporting documentation
and a copy of your claim to the address listed at the bottom of this form. Questions regarding a
submission should be directed to Claims Inquiry/Claims Research at 800-566-6444. Please use
one form per member.
Date:
MEMBER INFORMATION
Member Name
Date of Service
Patient Account No.
Billed Amount
Member ID
Claim Number
PROVIDER INFORMATION
Provider Name
Tax ID Number
Practice Name
NPI Number
Street Address
Fax Number
City/State/Zip
Contact name
Provider Phone No.
Contact Number
SUBMISSION INFORMATION (See second page for detailed descriptions)
Claim Reconsideration
Examples of Appeals
•
Prior-Authorization Appeal
Itemized Bill
•
Level of Care Appeal
Duplicate Claim
•
Medical Necessity Appeal
Corrected Claim (note “corrected” on claim)
•
Payment Dispute
Coordination of Benefits (note “corrected” on
•
Untimely Filing Appeal
claim)
•
Claim/Coding Edit Appeal
Proof of Timely Filing
•
Other Appeal Request
If any of the above apply, please do not use this
Claim/Coding Reconsideration
form and fax or mail the Appeal and all supporting
Other Claim reconsideration
documentation clearly marked as “Filing an
Appeal” to:
If you checked a box above, please mail claim and
Aetna Better Health of Missouri
all supporting documentation to:
Attn: Appeals
Aetna Better Health of Missouri
10 S. Broadway, Ste. 1200
P.O. 65855
St. Louis, MO 63102
Phoenix, AZ 85082
-
or -
Fax: 844-692-5109
MO-15-04-78
Form code: PARF
Revised 7/29/2015
 1
1 2
2