Vision Services Claim Form - 2011
ADVERTISEMENT
O
u
t
o
f
N
e
t
w
o
r
k
O
u
t
o
f
N
e
t
w
o
r
k
V
i
s
i
o
n
S
e
r
v
i
c
e
s
C
l
a
i
m
F
o
r
m
V
i
s
i
o
n
S
e
r
v
i
c
e
s
C
l
a
i
m
F
o
r
m
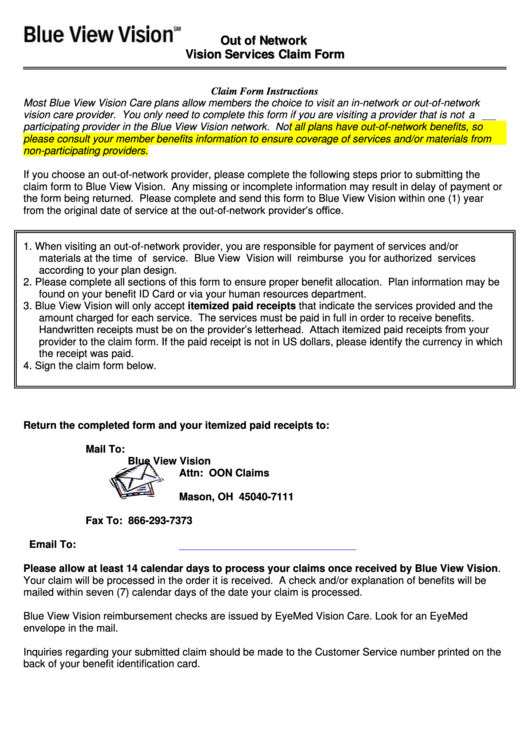
Claim Form Instructions
Most Blue View Vision Care plans allow members the choice to visit an in-network or out-of-network
vision care provider. You only need to complete this form if you are visiting a provider that is not a
participating provider in the Blue View Vision network. Not all plans have out-of-network benefits, so
please consult your member benefits information to ensure coverage of services and/or materials from
non-participating providers.
If you choose an out-of-network provider, please complete the following steps prior to submitting the
claim form to Blue View Vision. Any missing or incomplete information may result in delay of payment or
the form being returned. Please complete and send this form to Blue View Vision within one (1) year
from the original date of service at the out-of-network provider’s office.
1. When visiting an out-of-network provider, you are responsible for payment of services and/or
materials at the time of service.
Blue View Vision will reimburse you for authorized services
according to your plan design.
2. Please complete all sections of this form to ensure proper benefit allocation. Plan information may be
found on your benefit ID Card or via your human resources department.
3. Blue View Vision will only accept itemized paid receipts that indicate the services provided and the
amount charged for each service. The services must be paid in full in order to receive benefits.
Handwritten receipts must be on the provider’s letterhead. Attach itemized paid receipts from your
provider to the claim form. If the paid receipt is not in US dollars, please identify the currency in which
the receipt was paid.
4. Sign the claim form below.
Return the completed form and your itemized paid receipts to:
Mail To:
Blue View Vision
Attn: OON Claims
P.O. Box 8504
Mason, OH 45040-7111
Fax To:
866-293-7373
Email To:
Please allow at least 14 calendar days to process your claims once received by Blue View Vision.
Your claim will be processed in the order it is received. A check and/or explanation of benefits will be
mailed within seven (7) calendar days of the date your claim is processed.
Blue View Vision reimbursement checks are issued by EyeMed Vision Care. Look for an EyeMed
envelope in the mail.
Inquiries regarding your submitted claim should be made to the Customer Service number printed on the
back of your benefit identification card.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1 2
2 3
3








