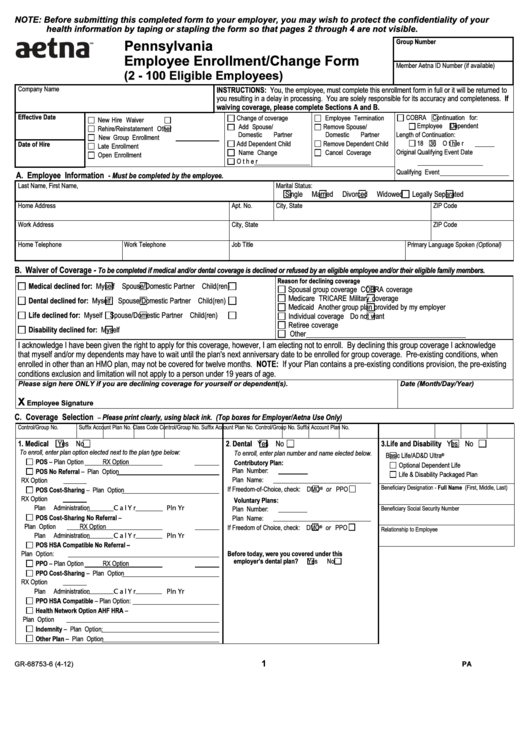
NOTE: Before submitting this completed form to your employer, you may wish to protect the confidentiality of your
health information by taping or stapling the form so that pages 2 through 4 are not visible.
Pennsylvania
Group Number
Employee Enrollment/Change Form
Member Aetna ID Number (if available)
(2 - 100 Eligible Employees)
Company Name
INSTRUCTIONS: You, the employee, must complete this enrollment form in full or it will be returned to
you resulting in a delay in processing. You are solely responsible for its accuracy and completeness. If
waiving coverage, please complete Sections A and B.
Effective Date
COBRA
Continuation for:
Change of coverage
Employee Termination
New Hire
Waiver
Employee
Dependent
Add Spouse/
Remove Spouse/
Rehire/Reinstatement
Other
Domestic Partner
Domestic Partner
Length of Continuation:
New Group Enrollment
18
36
Other
Add Dependent Child
Remove Dependent Child
Date of Hire
Late Enrollment
Original Qualifying Event Date
Name Change
Cancel Coverage
Open Enrollment
Other
Qualifying Event
A. Employee Information
- Must be completed by the employee.
Last Name, First Name, M.I.
Marital Status:
Single
Married
Divorced
Widowed
Legally Separated
Home Address
Apt. No.
City, State
ZIP Code
Work Address
City, State
ZIP Code
Home Telephone
Work Telephone
Job Title
Primary Language Spoken (Optional)
B. Waiver of Coverage -
To be completed if medical and/or dental coverage is declined or refused by an eligible employee and/or their eligible family members.
Reason for declining coverage
Medical declined for:
Myself
Spouse/Domestic Partner
Child(ren)
Spousal group coverage
COBRA coverage
Medicare
TRICARE Military coverage
Dental declined for:
Myself
Spouse/Domestic Partner
Child(ren)
Medicaid
Another group plan provided by my employer
Life declined for:
Myself
Spouse/Domestic Partner
Child(ren)
Individual coverage
Do not want
Retiree coverage
Disability declined for:
Myself
Other
I acknowledge I have been given the right to apply for this coverage, however, I am electing not to enroll. By declining this group coverage I acknowledge
that myself and/or my dependents may have to wait until the plan's next anniversary date to be enrolled for group coverage. Pre-existing conditions, when
enrolled in other than an HMO plan, may not be covered for twelve months. NOTE: If your Plan contains a pre-existing conditions provision, the pre-existing
conditions exclusion and limitation will not apply to a person under 19 years of age.
Date (Month/Day/Year)
Please sign here ONLY if you are declining coverage for yourself or dependent(s).
X
Employee Signature
C. Coverage Selection
Please print clearly, using black ink. (Top boxes for Employer/Aetna Use Only)
–
Control/Group No.
Suffix
Account
Plan No.
Class Code
Control/Group No.
Suffix
Account
Plan No.
Control/Group No.
Suffix
Account
Plan No.
1. Medical
Yes
No
2
Dental
Yes
No
3. Life and Disability
Yes
No
.
To enroll, enter plan option elected next to the plan type below:
To enroll, enter plan number and name elected below.
®
Basic Life/AD&D Ultra
POS – Plan Option
RX Option
Contributory Plan:
Optional Dependent Life
Plan Number:
POS No Referral – Plan Option
Life & Disability Packaged Plan
RX Option
Plan Name:
Beneficiary Designation - Full Name (First, Middle, Last)
®
If Freedom-of-Choice, check:
DMO
or
PPO
POS Cost-Sharing – Plan Option
RX Option
Voluntary Plans:
CalYr
Pln Yr
Plan Administration
Plan Number:
Beneficiary Social Security Number
POS Cost-Sharing No Referral –
Plan Name:
Plan Option
RX Option
®
If Freedom of Choice, check:
DMO
or
PPO
Relationship to Employee
Plan Administration
CalYr
Pln Yr
POS HSA Compatible No Referral –
Plan Option:
Before today, were you covered under this
employer’s dental plan?
Yes
No
PPO – Plan Option
RX Option
PPO Cost-Sharing – Plan Option
RX Option
Plan Administration
CalYr
Pln Yr
PPO HSA Compatible – Plan Option:
Health Network Option AHF HRA –
Plan Option
Indemnity – Plan Option:
Other Plan – Plan Option
1
GR-68753-6 (4-12)
PA
R-POD A
 1
1 2
2 3
3 4
4