Medical History Information Sheet
Download a blank fillable Medical History Information Sheet in PDF format just by clicking the "DOWNLOAD PDF" button.
Open the file in any PDF-viewing software. Adobe Reader or any alternative for Windows or MacOS are required to access and complete fillable content.
Complete Medical History Information Sheet with your personal data - all interactive fields are highlighted in places where you should type, access drop-down lists or select multiple-choice options.
Some fillable PDF-files have the option of saving the completed form that contains your own data for later use or sending it out straight away.
ADVERTISEMENT
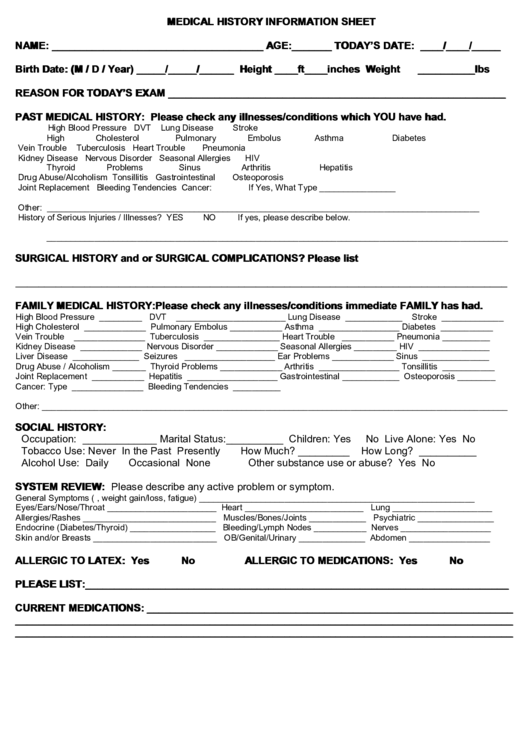
MEDICAL HISTORY INFORMATION SHEET
NAME: _____________________________________ AGE:_______ TODAY’S DATE: ____/____/_____
Birth Date: (M / D / Year) _____/_____/______
Height ____ft____inches
Weight __________lbs
REASON FOR TODAY’S EXAM ___________________________________________________________
PAST MEDICAL HISTORY: Please check any illnesses/conditions which YOU have had.
High Blood Pressure
DVT
Lung Disease
Stroke
High Cholesterol
Pulmonary Embolus
Asthma
Diabetes
Vein Trouble
Tuberculosis
Heart Trouble
Pneumonia
Kidney Disease
Nervous Disorder
Seasonal Allergies
HIV
Thyroid Problems
Sinus
Arthritis
Hepatitis
Drug Abuse/Alcoholism
Tonsillitis
Gastrointestinal
Osteoporosis
Joint Replacement
Bleeding Tendencies
Cancer:
If Yes, What Type ________________
Other: ___________________________________________________________________________________________
History of Serious Injuries / Illnesses? YES
NO
If yes, please describe below.
_________________________________________________________________________________________________
SURGICAL HISTORY and or SURGICAL COMPLICATIONS? Please list
______________________________________________________________________________________
FAMILY MEDICAL HISTORY: Please check any illnesses/conditions immediate FAMILY has had.
High Blood Pressure _________ DVT _______________________
Lung Disease ____________
Stroke _____________
High Cholesterol _____________ Pulmonary Embolus ___________
Asthma _________________ Diabetes ___________
Vein Trouble
_______________ Tuberculosis ________________
Heart Trouble
___________ Pneumonia __________
Kidney Disease _____________ Nervous Disorder _____________
Seasonal Allergies _________ HIV _______________
Liver Disease
______________ Seizures ___________________
Ear Problems _____________ Sinus ______________
Drug Abuse / Alcoholism _______ Thyroid Problems _____________
Arthritis _________________ Tonsillitis ___________
Joint Replacement ___________ Hepatitis ___________________
Gastrointestinal ____________ Osteoporosis ________
Cancer: Type _______________ Bleeding Tendencies __________
Other: __________________________________________________________________________________________________
SOCIAL HISTORY:
Occupation: _____________ Marital Status:__________ Children: Yes
No
Live Alone: Yes
No
Tobacco Use: Never
In the Past
Presently
How Much? _________
How Long? __________
Alcohol Use: Daily
Occasional
None
Other substance use or abuse? Yes
No
SYSTEM REVIEW: Please describe any active problem or symptom.
General Symptoms (i.e. fever, weight gain/loss, fatigue) __________________________________________________________
Eyes/Ears/Nose/Throat _______________________
Heart _________________________
Lung _____________________
Allergies/Rashes ____________________________
Muscles/Bones/Joints ____________
Psychiatric ________________
Endocrine (Diabetes/Thyroid) __________________
Bleeding/Lymph Nodes ___________
Nerves ___________________
Skin and/or Breasts __________________________
OB/Genital/Urinary ______________
Abdomen _________________
ALLERGIC TO LATEX: Yes
No
ALLERGIC TO MEDICATIONS: Yes
No
PLEASE LIST:__________________________________________________________________________
CURRENT MEDICATIONS: ________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1








