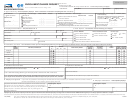
Instructions
A. Complete a claim form.
Most providers will bill directly for you and no claim form will be necessary. However, if you do incur
expenses from a provider who will not bill the plan directly, you will need to complete a claim form and provide an itemized bill. (See
section B for information about itemized bills.)
B. Attach the itemized bill.
Please do not highlight or modify the itemized bill as this may cause delayed processing of your claim.
The itemized bill must contain all of the following information:
• Name of the member who incurred the expense.
• Name, address, and IRS tax identification number of the provider.
• Diagnosis code (ICD-10). This information must be obtained from your provider.
• Procedure codes (CPT-4, HCPCS, ADA, or UB-04). This information must be obtained from your provider.
• Date of service and itemized charge for each service rendered.
Please note: Your claim will be returned if all of the required information listed above is not included.
C. The front of your member ID card
may not match the card pictured below. This sample card is meant to be a guide to help you
identify your prefix, identification, and group numbers. These numbers are required to complete your claim form.
1
2
1 — Prefix and Identification #
help us verify your eligibility, determine your
coverage, and process claims.
2 — Group #
identifies your plan’s benefits.
D. The back of your member ID card
provides additional information. To help ensure your claims are paid properly, encourage
physicians and other providers to copy the front and back of your card each time you visit.
You can research claim and eligibility information online. Visit our self-service website at . You may also call Customer
Service at the phone number shown on the back of your ID card.
 1
1 2
2