Medication Prior Authorization Form
ADVERTISEMENT
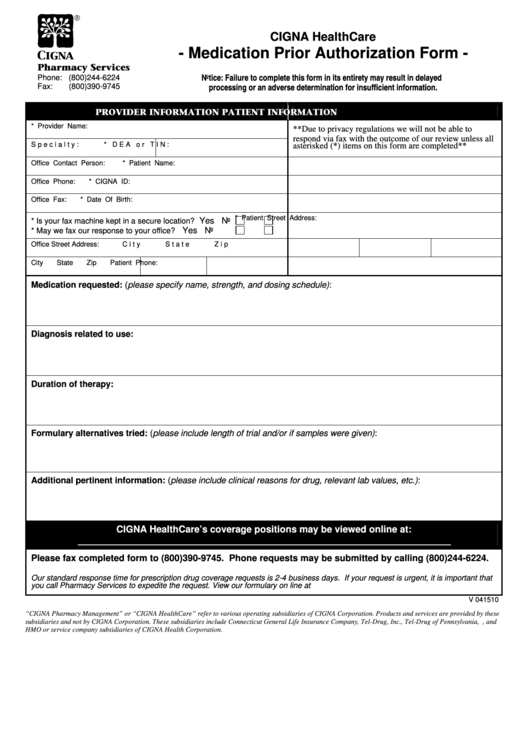
CIGNA HealthCare
- Medication Prior Authorization Form -
Pharmacy Services
Notice: Failure to complete this form in its entirety may result in delayed
Phone: (800)244-6224
processing or an adverse determination for insufficient information.
Fax:
(800)390-9745
PROVIDER INFORMATION
PATIENT INFORMATION
* Provider Name:
**Due to privacy regulations we will not be able to
respond via fax with the outcome of our review unless all
Specialty:
* DEA or TIN:
asterisked (*) items on this form are completed**
Office Contact Person:
* Patient Name:
Office Phone:
* CIGNA ID:
Office Fax:
* Date Of Birth:
* Patient Street Address:
Yes
No
* Is your fax machine kept in a secure location?
Yes
No
* May we fax our response to your office?
Office Street Address:
City
State
Zip
City
State
Zip
Patient Phone:
Medication requested: (please specify name, strength, and dosing schedule):
Diagnosis related to use:
Duration of therapy:
Formulary alternatives tried: (please include length of trial and/or if samples were given):
Additional pertinent information: (please include clinical reasons for drug, relevant lab values, etc.):
CIGNA HealthCare’s coverage positions may be viewed online at:
Please fax completed form to (800)390-9745. Phone requests may be submitted by calling (800)244-6224.
Our standard response time for prescription drug coverage requests is 2-4 business days. If your request is urgent, it is important that
you call Pharmacy Services to expedite the request. View our formulary on line at
V 041510
“CIGNA Pharmacy Management” or “CIGNA HealthCare” refer to various operating subsidiaries of CIGNA Corporation. Products and services are provided by these
subsidiaries and not by CIGNA Corporation. These subsidiaries include Connecticut General Life Insurance Company, Tel-Drug, Inc., Tel-Drug of Pennsylvania, L.L.C., and
HMO or service company subsidiaries of CIGNA Health Corporation.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1








